Dka icu Management
- Category Diabetes Freedom
- Tag: Product
Price:
$37
$197
-

Delivery
Worldwide coverage or instant download to your computer -

Product
Guaranteed 100% genuine
good quality -

Bill
Provide invoice
Share
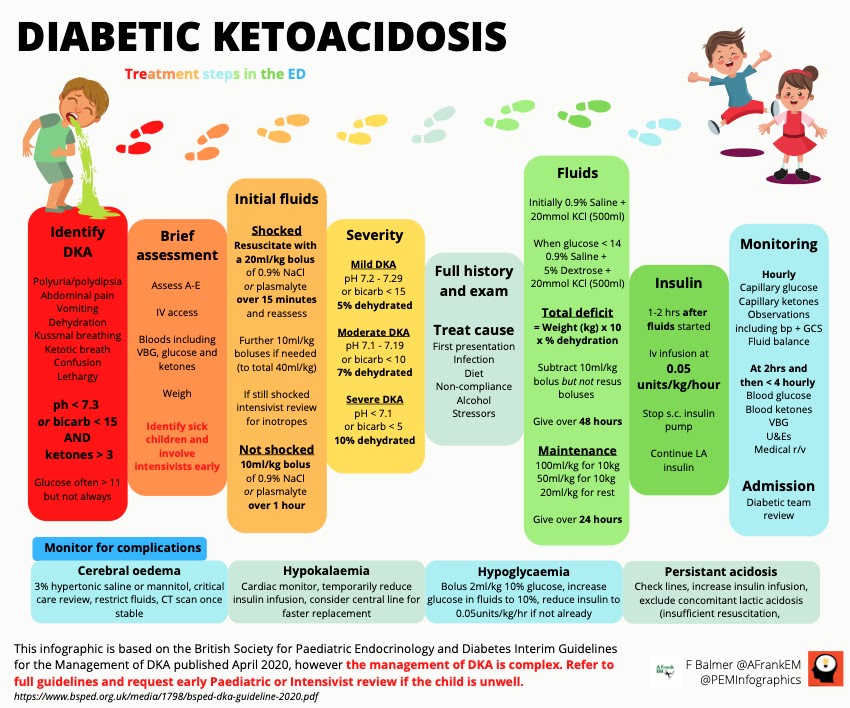
DKA, or diabetic ketoacidosis, is a life-threatening emergency that requires immediate treatment. Left untreated, DKA can lead to coma and death. The mainstay of treatment for DKA is intravenous insulin therapy.
Intravenous insulin therapy is very effective at reversing the symptoms of DKA. It works by lowering the blood sugar and preventing the build-up of ketones in the blood. Intravenous insulin therapy is typically given in an intensive care setting, where close monitoring can ensure that the patient's blood sugar remains within a safe range.
Intravenous insulin therapy can be a challenge to administer, but with careful monitoring it can be a safe and effective way to treat DKA.
Dka icu management - Management of adult diabetic ketoacidosis:
Diabetic Ketoacidosis (DKA)
Causes
Symptoms
Some of the symptoms that people experience with DKA include the following:
- Excessive thirst and urination (more water is pulled into the urine as a result of high ketone loss in the urine)
- Lethargy
- Breathing very quickly (patients have a very high level of acids in their bloodstream and they try to "blow" off carbon dioxide by breathing quickly)
- A fruity odor on their breath (ketones have a fruity smell)
- Nausea and vomiting (the body tries to get rid of acids any way it can-even stomach acid!)
- Confusion
- Blurred vision
- Decreased perspiration (in line with the excessive urination...patients are very dehydrated)
- Potassium: 5.5 (normal range: 3.5-5.5)
- Anion Gap: Unable to calculate (AKA greater than 30; normal range: 6-14)
- Glucose: 925 (normal range: 70-120)
- Magnesium: 1.6 (normal range:1.4-2.6)
- Phosphorus: 1.8 (normal range: 2.3-5.6)
- Bicarbonate (same as CO2 on a BMP): Less than 5 (normal range 20-30)
We are frequently monitoring the patient's electrolytes (usually every four hours) to be sure that they do not either get too high or too low. Remember that as insulin is used to pull sugar into the cells, potassium is also used at the same time! When a patient is severely hyperkalemic, doctors will sometimes order D50 (pretty much straight sugar) and insulin to be given because using insulin decreased potassium levels. Be sure not to bottom out your patient's potassium as you are normalizing their sugar. The electrolytes all work hand in hand so monitor magnesium and phosphorus as well.
The anion gap is a good judge of how well the DKA is resolving. The anion gap is calculated on your BMP. If you wanted to calculate it manually (which we never do), it is a measurement of the number of chloride and bicarbonate anions together subtracted from the number of sodium and potassium cations. You can see why it's a good measure because as your DKA resolves your electrolytes become more stable and your anion gap returns to normal.
The bicarbonate is also a good measurement of how the DKA is progressing. As your acid level rises in your body (due to the acidic ketones), the bicarbonate is used as a buffer to try and relieve some of the acidity. This depletes the bicarbonate. Sometimes in severe cases of DKA the doctors will put the patients on a bicarbonate IV drip to try and help neutralize the patient's acids. The patient will naturally try and expel extra acids by breathing quickly and blowing off carbion dioxide (which is an acid). Their venous blood gas is going to be UGLY! An example is as follows: pH 7.06, pCO2 20, and bicarb 5. UGLY! Don't freak out though. This will resolve as the ketones are expelled and the bicarb increases.
As the patient recovers from DKA, the anion gap will decrease and the bicarbonate will increase. The patient's sugar will begin to resolve as you give insulin and everything else usually follows suit. Once the blood sugar has resolved, we usually supplement the patient's IV fluids with D5. The maintenance fluid of choice is generally Lactated Ringers at 200 mL/hr until the blood sugar reaches less than 200; then we change the fluid over to D5/LR. The IV insulin helps with resolving the DKA so we supplement with sugar to continue the insulin until the DKA is finished. Once the labs have resolved, we give Lantus (long-acting insulin) about 3-4 hours before we discontinue the insulin drip. Patients are usually feeling much better at this point and get transfer orders for a general medical unit.






Post a Comment